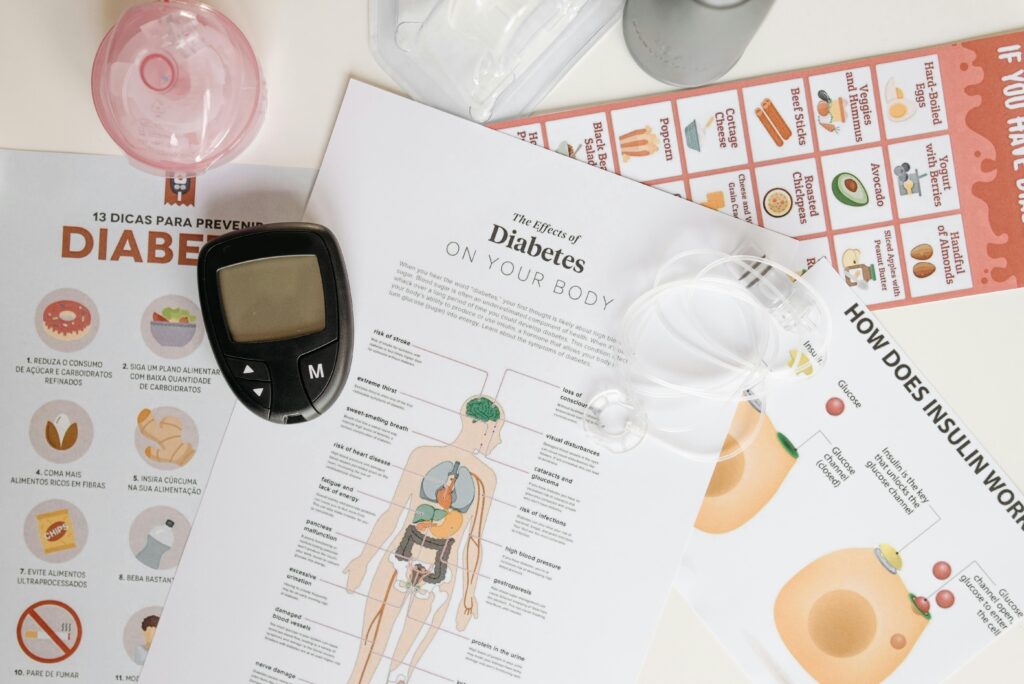
Living with diabetes is not always easy, especially as we grow older. The day starts with tablets, continues with meal planning, and ends with checking sugar levels. It feels like one long balancing act. Most of us try our best to follow the doctor’s advice, but sometimes small mistakes slip in without us realising.
These little mistakes may not cause a problem immediately, but over months and years, they can affect how well our medicine works. And when medicines don’t work the way they should, sugar levels start going up and down, leaving us tired, confused, and frustrated.
The good news is that most of these mistakes are easy to fix. Once we know what to watch out for, managing diabetes becomes much simpler and safer.
Here are the 7 common mistakes seniors make while taking diabetes medicine—and how we can avoid them.
1. Skipping Meals but Still Taking Medicine
Many elders skip breakfast because they don’t feel hungry. Some skip dinner thinking it will help with weight loss. But the medicines keep working in the body even when food is not there. This can drop sugar levels dangerously low.
Symptoms include:
- sweating
- trembling
- dizziness
- sudden weakness
- confusion
- irritability
Low sugar can be more dangerous than high sugar for older adults. A single fall caused by fainting can change life forever.
How to avoid this mistake
- Never skip meals, especially breakfast.
- If appetite is low, eat something light—idli, a small bowl of oats, milk, fruits, or a handful of nuts.
- If you genuinely cannot eat, tell your doctor so they can adjust your dosage.
Food is fuel. Medicine works best when it has something to work with.
2. Taking the Wrong Dose—or Taking It at the Wrong Time
This happens more often than we admit. As medicines increase over the years, it becomes harder to track which tablet to take when. Many elders accidentally:
- take two doses
- forget a dose
- take morning tablets at night
- take night tablets in the afternoon
- mix up insulin units
These errors can cause sugar swings, weakness, and emergencies.
How to avoid this mistake
- Use a weekly pill organizer.
- Set alarms on your phone.
- Keep morning and night tablets in separate boxes.
- Mark insulin pens clearly.
- Ask a family member to check once a week.
A little organisation protects us from big troubles.
3. Adjusting the Dose on Our Own
We all do this at some point. We feel sugar is “normal,” so we think we can reduce the dose. Or when sugar is high one morning, we think taking extra tablets will control it faster.
Sadly, it doesn’t work like that. Diabetes medicines need steady, consistent dosing. Changing it suddenly can:
- damage kidneys
- cause severe lows
- cause dehydration
- weaken the heart
- affect eyesight
- create big fluctuations
Only a doctor knows how to adjust safely.
How to avoid this mistake
We should never increase or decrease doses on our own—even if sugar is high or low. Instead:
- Take a picture of the reading.
- Note what you ate, how well you slept, and any stress.
- Share it with your doctor.
- Let them guide the change.
Trust the prescription, not the panic.
4. Mixing Diabetes Medicine With Home Remedies Without Checking
Many of us try herbal remedies—fenugreek water, neem, karela juice, cinnamon, turmeric milk, jamun seed powder, and so on. These can be helpful in moderation. But when combined with diabetes tablets, some remedies can push sugar levels too low.
Some home remedies also affect the kidneys or react with other medicines like blood thinners and blood pressure tablets.
How to avoid this mistake
- Don’t try too many remedies at once.
- Talk to your doctor before adding anything new.
- Try one remedy at a time and monitor sugar carefully.
- Avoid extreme remedies like bitter herbal concoctions on an empty stomach.
Natural is good—but safe is better.
5. Taking Medicines With Tea or Coffee
It is a habit many of us have: pop the morning tablet with the first cup of tea or coffee.
But caffeine slows down how some medicines work. Filters coffee and strong tea can also irritate the stomach and cause acidity, which affects absorption.
Certain medicines need an empty stomach. Others need food. Tea or coffee is neither.
How to avoid this mistake
- Take medicines with water—not tea or coffee.
- Follow meal instructions carefully.
- Have tea or coffee 20–30 minutes after medicines if needed.
It is a small habit change with big benefits.
6. Not Drinking Enough Water Throughout the Day
Body water reduces with age. Many seniors avoid drinking water because of increased urination, joint pain, or fear of going to the bathroom at night.
But dehydration can make diabetes medicines (especially metformin or tablets for the kidneys) harder on the body. It can also make sugar levels appear higher than they actually are.
Symptoms of dehydration include:
- dry mouth
- headache
- constipation
- dark urine
- fatigue
Older adults may not even feel thirsty, but the body still needs water.
How to avoid this mistake
- Sip water slowly throughout the day instead of drinking large amounts at once.
- Keep a small bottle next to the bed or chair.
- Drink more in the daytime and less after 7 pm to avoid night trips to the bathroom.
- Add soups, coconut water (unsweetened), buttermilk, and fruits with water content.
Hydration keeps medicines gentle on the body.
7. Forgetting That Lifestyle Is Also Part of the Treatment
Many seniors rely only on tablets or insulin and ignore lifestyle changes.
But diabetes medicine works best when supported by:
- regular walking
- balanced meals
- portion control
- good sleep
- light physical activity at home
- stress reduction
Some elders eat high-sugar foods thinking “medicine will take care of it.”
Some avoid walking due to fear of falls.
Some sleep late and wake late, which disrupts sugar rhythms.
Medicines can only do so much. The real magic happens when medicines and habits work together.
How to avoid this mistake
- Walk for 10–15 minutes after meals—inside or outside the house.
- Eat smaller, more frequent meals if digestion is slow.
- Avoid heavy rice portions at night.
- Go to bed and wake up at regular times.
- Stretch gently every morning.
Small steps add up, even at 60, 70, or 80.
Bonus Tip: Keep Your Doctor Updated Regularly
Many of us visit the doctor only when something goes wrong. But diabetes changes with age, diet, stress levels, sleep, and overall health. Medicine doses that worked last year may not be right today.
A quick update every 3–4 months can prevent complications and catch early issues like:
- kidney stress
- nerve problems
- eye changes
- sudden sugar shifts
- thyroid imbalance
- blood pressure changes
Regular check-ins keep treatment safe and effective.
Final Thoughts
Diabetes is a condition that needs patience, understanding, and routine. As we age, that routine becomes even more important. The goal is not to live in fear of medicine, but to use it wisely and safely. When we avoid these common mistakes and stay consistent with healthy habits, life becomes smoother, sugar levels stay more stable, and we feel more confident about our health.
If you found these insights helpful, we would love to hear your experiences.
Share your thoughts, your questions, or any lessons you’ve learned about managing diabetes medicines. And if this blog can help a friend, neighbour, or family member, do share it with them too.