Recovering from a stroke is a journey—slow, steady, and deeply personal. With the right routines at home, patient guidance from family, and timely medical follow-up, stroke survivors can regain confidence and independence.
What a stroke is (in simple words)
A stroke happens when blood flow to a part of the brain stops or a vessel bursts. It can affect movement, speech, memory, vision, mood, and swallowing. Quick treatment saves brain cells and improves recovery. Remember F.A.S.T. for warning signs: Face drooping, Arm weakness, Speech difficulty—Time to get emergency help.
If you notice new F.A.S.T. symptoms in a survivor, treat it as an emergency—strokes can recur.
The first 90 days: why they matter
The first few months after a stroke are critical for rehabilitation—physio, speech therapy, occupational therapy, and emotional support. Consistent practice during this window often leads to better long-term outcomes.
Setting up the home for safety and recovery
1) Prevent falls and make movement easier
- Clear clutter, secure loose wires and rugs.
- Install grab bars in bathroom; use non-slip mats.
- Keep a sturdy chair with arms for easy sitting/standing.
- Ensure good lighting at night (bedroom → bathroom path).
2) Support mobility and exercises
- Follow a physiotherapist-prescribed exercise plan (range-of-motion, balance, walking practice).
- Short, frequent sessions are better than one long session.
- Use walking aids only if advised (cane, walker).
Research from India highlights the need to train caregivers in safe home exercises to reduce strain and improve outcomes.
3) Safer eating and swallowing (if dysphagia)
- Sit upright during meals and for 30–45 minutes after.
- Take small bites/sips; avoid distractions while eating.
- Use texture-modified diets (soft/mashed/thickened) if the therapist advises.
- Watch for coughing while eating, wet/gurgly voice, or repeated chest infections—tell the doctor.
4) Prevent bedsores
- Turn the person every 2 hours if bed-bound.
- Use cushions/air mattresses if recommended.
- Keep skin clean and dry; moisturize dry areas.
5) Hand and shoulder care
- Support the weak arm while sitting/walking.
- Avoid pulling the arm during transfers (risk of shoulder injury).
- Gentle, guided stretching to prevent stiffness.
Daily routine that helps
Morning
- Vitals check if advised (BP, sugar).
- Personal hygiene with adaptive tools (long-handled sponge, shower chair).
- Short exercise block (mobility + balance).
Midday
- Speech practice (naming objects, reading aloud), memory games, simple chores.
Evening
- Walk (indoors or outdoors if safe), breathing exercises, light stretching.
- Wind-down ritual: music, prayer, meditation.
High-quality, goal-oriented rehab—at home or in structured programs—improves independence when patients and families work as a team.
Nutrition the Indian way
- Focus on fresh vegetables, dals, sprouts, whole grains (millets, brown rice, chapati), fruits, and adequate protein (paneer, curd, eggs, fish if non-veg).
- Limit salt (helps BP control), sugar, and deep-fried foods.
- Heart-healthy oils (mustard/groundnut/sunflower) in moderation.
- Adequate water unless fluid restricted by the doctor.
- If swallowing is difficult, try soft khichdi, dalia, curd rice, well-cooked veg, thick soups—guided by the therapist.
Medications & monitoring
- Keep a medication chart; use pill organizers/phone reminders.
- Never stop blood thinners, BP, sugar, or cholesterol medicines without medical advice.
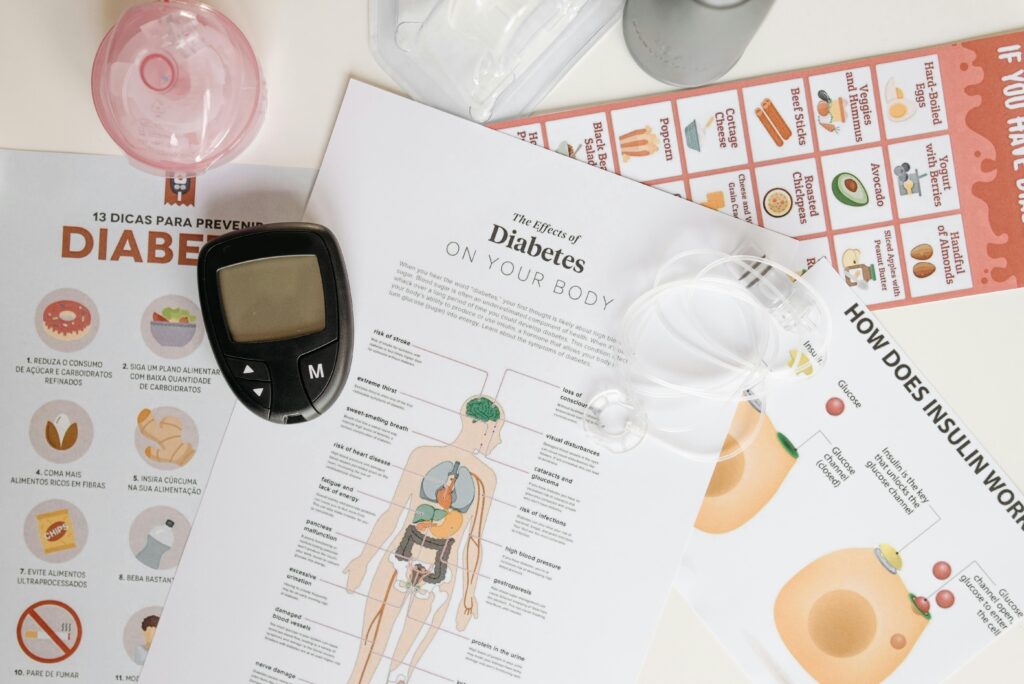
- Track BP, blood sugar (if diabetic), weight, and any new symptoms; show records at reviews.
Evidence-based guidelines stress long-term risk control to prevent another stroke.
Communication after stroke (aphasia)
- Use short sentences and speak slowly.
- Ask yes/no questions; give time to respond.
- Use pictures, gestures, and writing boards.
- Celebrate small wins—one new word, one longer phrase.
Emotions & mental health
Low mood, anxiety, irritability, and fatigue are common. Normalize feelings, encourage routine, sunlight, social time, and enjoyable activities. If sadness, sleep loss, or hopelessness persist, consult the doctor—treating post-stroke depression improves rehab participation and recovery.
Helping the caregiver
- Learn safe transfer techniques from the therapist.
- Set realistic weekly goals (e.g., 20-meter walk, buttoning a shirt).
- Use respite: share duties among family, consider day-care/short-term help.
- Keep emergency contacts and a hospital file ready.
A Chennai study showed that structured caregiver training at discharge is vital for effective home-based rehab.
Preventing another stroke
- Control BP, sugar, cholesterol; take medicines regularly.
- Stop smoking and avoid alcohol.
- Move daily; maintain a healthy weight and good sleep.
- Keep follow-up appointments with neurology/physiatry/therapy teams.
- Know the F.A.S.T. signs and act immediately if they reappear.
When to seek urgent care
- New or worsening weakness/numbness on one side.
- Sudden trouble speaking, understanding, or seeing.
- Severe headache with vomiting.
- Sudden loss of balance or fainting.
Don’t wait—time is brain.
Useful Indian resources
- Indian Stroke Association – professional information and awareness.
- Caregiver-friendly guidelines (India) – summaries and pointers for prevention/management.
Gentle reminder
This guide is for education, not a substitute for medical advice. Please follow your doctor and therapists’ personalized plan.
💬 Tell us what works for you!
Do you care for a stroke survivor at home? What routines, tools, or tips helped the most?
👉 Share your story in the comments to help other families.
📢 If you found this useful, share this blog with friends and support groups—your share could make someone’s recovery easier.